Gaining insurance credentialing is one of the most essential steps in building a successful practice as a mental health provider. The process allows you to become an approved provider with insurance companies, enabling you to offer services to clients with insurance coverage. It also involves a thorough examination of a provider’s credentials, background, and reputation to ensure they satisfy the standards established by insurance companies. Although it seems complicated and time-consuming, medical credentialing is essential for growing your audience and guaranteeing consistent income.
We will review everything you need to know in this comprehensive guide to help you get accepted by insurance companies.

Expand your client base
Many individuals rely on their insurance benefits for mental health services, limiting their options to in-network providers.
Increase Revenue
Accepting insurance can lead to a more constant and predictable income source.
Enhance credibility
Being credentialed can demonstrate your qualifications and professionalism to your clients.
Simplify billing
You can streamline the medical billing process by dealing directly with insurance companies.
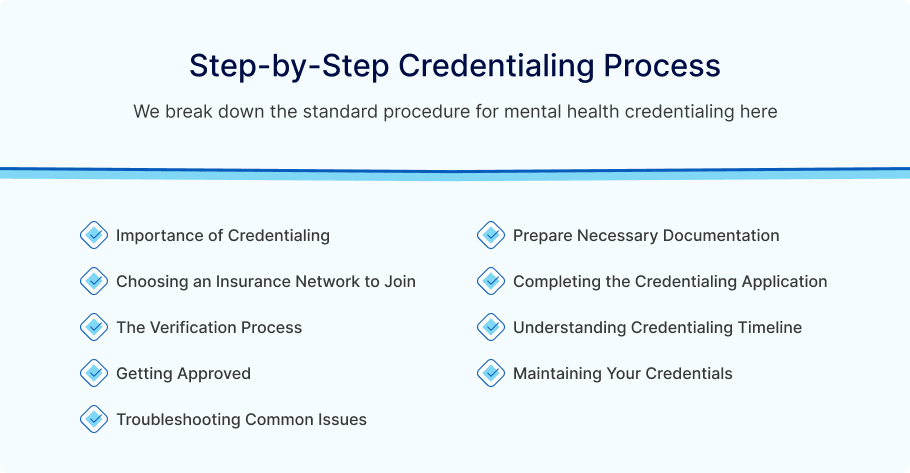
Importance of Credentialing
Before Beginning the Process, it is essential to comprehend the significance of certification. Being credentialed with insurance providers has benefits, including better revenue flow and the opportunity to provide services to insured individuals.
Prepare Necessary Documentation
The most crucial step in credentialing is ensuring you have all the necessary documents. This section needs your license, education verifications, malpractice insurance, and tax ID.
Choosing an Insurance Network to Join
All insurance companies do not work on the same platform. Consider the benefits each insurance provider offers and the type of clients you want to serve to determine which insurance network you want to join.
Completing the Credentialing Application
Insurance companies typically require providers to complete comprehensive applications. This section explains what to expect in the application, how to complete it, and common mistakes to avoid.
The Verification Process
The insurance company will start checking your credentials after you submit your application. In this, we cover how long the procedure usually takes, what factors cause delays, and how to stay proactive during the waiting period.
Understanding Credentialing Timeline
Establishing reasonable expectations regarding the duration of the credentialing procedure is critical. This includes defining the regular timetable and identifying any factors that could speed up or slow down the process.
Getting Approved
Once you have received the credentials, you are almost there. The following steps are to get listed in insurance directories, establish contracts with insurance companies, and negotiate reimbursement rates.
Maintaining Your Credentials
Once approved, it is important to maintain your credentials, which includes renewing the Process, keeping all the information up to date, and knowing what to do if the procedure changes.
Troubleshooting Common Issues
The credentialing procedure may present difficulties despite your best efforts. In this section, you will go through frequent problems, including denials, rejections, and delayed applications.
What is Mental Health Credentialing?
Mental health credentialing is the Process through which mental health professionals such as psychologists, counselors, therapists, social workers, and psychiatrists are formally recognized and approved by insurance companies to bill for services provided to covered customers. This procedure involves verifying providers’ qualifications, including license, professional experience, and adherence to industry standards.
Why is Mental Health Credentialing Important?
Credentials with insurance providers are essential for mental health professionals who want to expand their practices and ensure a steady stream of clients. Providers may be unable to serve insured clients if they lack the credentials necessary to accept insurance payments. Credentialing guarantees payment for your services, helps you demonstrate your credibility as a provider and fosters client trust.
Conclusion
Mental health credentialing is crucial for providers who want to grow their practices and work with insurance companies. By understanding the process and meeting the requirements, you can increase your client base and compensate for your work in the mental health field. Completing the insurance credentialing procedure is essential to creating a successful mental health practice. You can effectively finish the credentialing Process and start providing services to covered customers by ensuring your qualifications are in order and applications are correctly submitted. Suppose you prepare and pay more attention to the details.
In that case, credentialing can assist you in creating a successful, long-lasting practice that gives a more significant population access to essential mental health services.
Philadelphia Medical Billing Company is a valuable partner in the Mental Health Credentialing Process. The company has a team of experts to assist mental health providers in gathering the necessary documentation, completing applications, and ensuring that all forms are submitted accurately and on time. By handling the paperwork and communication with insurance companies, a medical billing company allows providers to do their best to deliver quality care.
Contact us today for adequate mental health credentialing.