Family medicine remains a cornerstone of primary care in the United States, offering comprehensive services across all age groups. As billing regulations become increasingly complex, 2025 will significantly impact how family medicine practices manage revenue. From updates to E/M codes and payer-specific rules and telehealth adjustments, staying compliant is crucial for maximizing reimbursements and avoiding denials.
This guide breaks down the latest changes from govt or commercial payers and billing strategies every family physician should understand and implement this year.
Current Billing Challenges faced by Family practices
Below are the top most important RCM (Revenue Cycle Management) roadblocks faced by family physicians. These are given below:
Regulatory Changes
Regulatory changes are significant in the financial aspects of service reimbursement for family medicine practices. Sometimes, you don’t follow or read the latest changes in healthcare regulation. Your claims get rejected only due to the unawareness of the modifications made by the payer or insurance providers.
Coding Changes
Billing for Family medicine physicians need to stay updated with the coding changes made by Medicare or any private insurer.
It usually happens when a new medical service or a procedure is added. It also requires a code and a modifier.
For example, due to the COVID-19 pandemic outbreak in 2019, Medicare and other payers introduced it as a new service/procedure. To enable providers to bill these services under defined policies.
To know the latest changes made by the payor, you must keep accessing the official coding resources and remain updated regarding any changes from the respective entity.
Top Family Medicine Billing Changes in 2025
Billing changes in family medicine occur due to shifting healthcare priorities like evolving care delivery models. For 2025, new advanced primary care management(APCM) codes to streamline and enhance chronic care reimbursement and increased use codes that reflect care complexity during office visits are some of the significant billing changes that CMS has implemented.
Let’s see some major highlights from CMS.
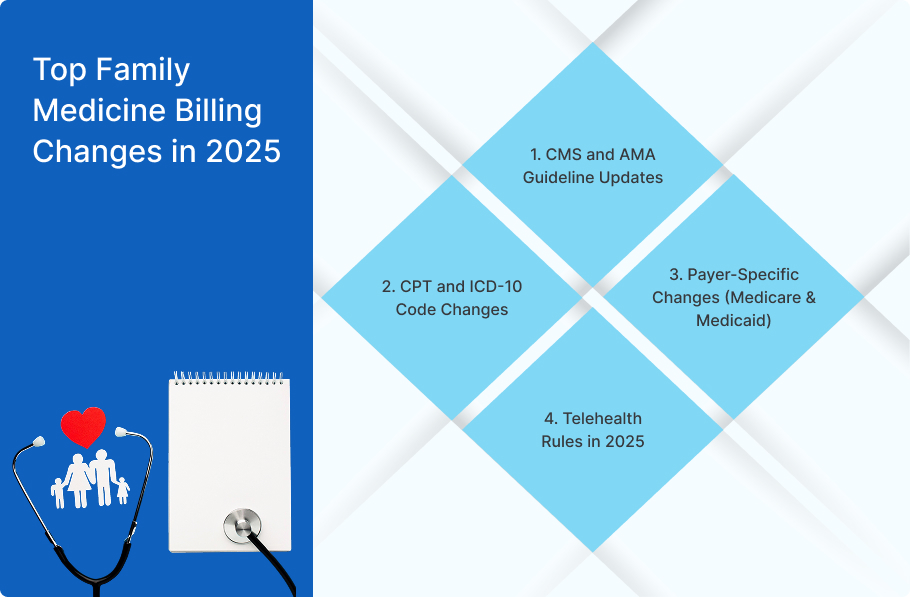
1. CMS and AMA Guideline Updates
CMS(Centers for Medicare & Medicaid Services) aligns more closely with AMA CPT criteria, especially for remote care and E/M coding. The Centres for Medicare & Medicaid Services(CMS) lowered the Medicare Conversion Factor by 2.9% to 2.93% for 2025, which affects family physician reimbursement rates.
When paid with modifier 25 on claims for Annual Wellness Visits, vaccinations, or other Medicare Part B preventive services, CMS will permit reimbursement for the G2211 Complexity add-on code.
Revised definitions and classifications affect how time and medical decision-making are documented.
2. CPT and ICD-10 Code Changes
New CPT codes support expanded remote monitoring and chronic care management. To record Advanced Primary Care Management(APCMA) services, which combine several current care management and communication technology-based services, CMS has added three new HCPCS codes. These codes aim to enhance supporting primary care models by identifying accurate procedures. Several ICD-10 updates address behavioral health and chronic condition classifications.
3. Payer-Specific Changes (Medicare & Medicaid)
Every insurance payor updates its guidelines when introducing a new code, procedure, or service. The physicians must remain updated with the internal changes payors make to ensure accurate claim processing.
For instance, Medicare has introduced stricter audits for long-term, chronic, and prolonged care visits. State-specific Medicare programs have updated telehealth policies and pre-authorization. States may alter Medicaid reimbursement guidelines in several ways, which could impact family doctors’ billing procedures. Keeping up with state-specific Medicare regulations is crucial.
4. Telehealth Rules in 2025
Many pandemic-era flexibilities have expired, especially those related to audio-only visits. When patients cannot use or refuse content with video technology, CMS has finalized the use of two-way, real-time audio-only communication for Medicare telehealth services. Real-time video is now often required for telehealth reimbursement, and geographic restrictions may apply in some states.
Evaluation & Management (E/M) Coding for Family Physicians
In 2025, Medicare urged family practice owners to utilize some essential E/M codes. These are:
Codes 99202–99215
These codes remain central to documenting in-office and outpatient visits. Family doctors should choose the correct E/M code (99202-99215) depending on the quality of care provided, considering variables including the patient’s condition’s complexity and the amount of time spent.
In 2025, documentation may be based on either total time (including face-to-face and certain non-face-to-face consultations with a patient for a specific service or a procedure or medical decision-making (MDM).
Time vs. MDM
In medical Coding, time and medical decision-making(MDM) are two different methods used to determine the level of service for evaluation and management (E/M) services.
Time-Based Coding: when a physician sees a patient and provides 50% counseling, coordination, or care coordination, he will utilize time-based Coding.
MDM-Based Coding: It is based on the number and complexity of problems addressed, data reviewed, and risk involved.
Tips for Accurate Level Selection
Here are some tips for Accurate level selection
Document Thoroughly: Record every aspect of the E/M service, including the history, examination, and medical treatment.
Use Appropriate Modifiers: Use modifier 25 when billing separately identifiable services performed on the same day.
Common Pitfalls and How to Avoid Downcoding
As telehealth becomes an increasingly integral part of healthcare delivery in 2025, providers and billing teams must navigate a complex and evolving regulatory landscape. Downloading in E/M coding occurs when a provider bills a lower-level service than what was performed, often due to incomplete documentation or misunderstanding of coding guidelines.
A common pitfall is failing to utilize the updated 2021/2023 E/M guidelines, which allow physicians to code based on either the complexity of medical decision-making (MDM) or the total time spent on the day of the encounter.
The amended 2021/2023 E/M standards, which enable doctors to code based on the complexity of medical decision-making (MDM) or the overall amount of time spent on the day of the encounter, are frequently overlooked.
Avoid Underreporting: Ensure that the level of service provided is accurately reflected in the selected code.
Comply with documentation Required: Follow the documentation instructions to support the service level that was billed.
Preventive vs. Problem-Oriented Visit Billing
Family physicians often manage preventive and problem-oriented care in the same visit, making distinguishing between the two for billing critical.
AWV and IPPE Services
Annual Wellness Visit (AWV) helps physicians develop or update a personalized prevention plan and perform a health risk assessment.
- Covered once every 12 months
- Patients pay nothing
Preventive Physical Examination (IPPE) enables doctors to review medical and social health history and preventive services education.
- New Medicare patients within 12 months
- Patients pay nothing
Modifier 25
Use Modifier 25 when a significant, separately identifiable problem-oriented service is performed on the same day as a preventive visit. Ensure clear, distinct documentation for both services to avoid claim rejections.
Chronic Care and Care Coordination Service
In the United States, family physicians often provide chronic care for long-term illnesses or conditions like diabetes or heart disease, so they must understand CCM codes.
Let’s have a look at the CCM codes below:
Chronic Care Management (CCM)
Chronic care management (CCM) service is essential for patients with multiple chronic conditions. The following CPT codes are used
CPT 99490: 20 minutes of non-face-to-face care coordination.
CPT 99439: Additional 20-minute
CPT 99491: 30 minutes of chronic care management
CPT 99487: At Least 60 minutes of complex chronic care management services for patients with moderate to complex conditions.
CPT 99489: Each additional 20 minutes of complex care management services.
Transition Care Management (TCM)
TCM services are reimbursed based on the complexity of the patient’s condition and the time spent coordinating care.
These services are provided to patients following a discharge from inpatient settings.
A physician needs to use the relevant CPT code for this service as:
CPT 99495 & 99496: For post-discharge services, based on time and contact type.
Behavioral Health Integration
In 2025, there’s increased support for collaborative care models, including more reimbursement opportunities. These services involve the integration of behavioral health care into primary care settings. The relevant CPT code is:
CPT 99848 20 minutes of BHI care.
Telehealth & Virtual Services Billing in 2025
In 2025, telehealth billing practices will continue to evolve by staying compliant with CMS guidelines and understanding new billing codes and reimbursement updates for telehealth services. Providers need to be aware of specific CPT/HCPCS codes and their effective dates and ongoing extensions of services like those for outpatient visits.
Approved CPT Codes
In 2025, CMS will not be using the new CPT telemedicine codes. Instead, in-person E/M codes with the relevant modifiers should be used to report telemedicine visits:
Modifier 95: A real-time interactive audio and video communications system provides synchronous telemedicine services via audio/video.
Modifier 93: For audio-only (synchronous telemedicine services delivered over the phone or through another interactive, real-time audio-only device).
Audio/Video Requirements
Most services now require real-time audio and video, like one-on-one or face-to-face doctor-patient consultations. CMS expects audio-visual technology unless the patient lacks video capability or declines video use. Audio-only visits are allowed in some situations, but the exception needs to be recorded.
Reimbursement Parity status
Parity status in telehealth reimbursement refers to the same payment for the telehealth services as for in-person services, which means a person who visits a doctor physically and a person who takes virtual consultation will pay the same fee for the services.
Payment parity for telehealth still varies by state and payer. While some states have enacted laws requiring private insurers to reimburse telehealth services at the same rate as in-person visits, others have not. Providers should check with individual payers to determine reimbursement rates.
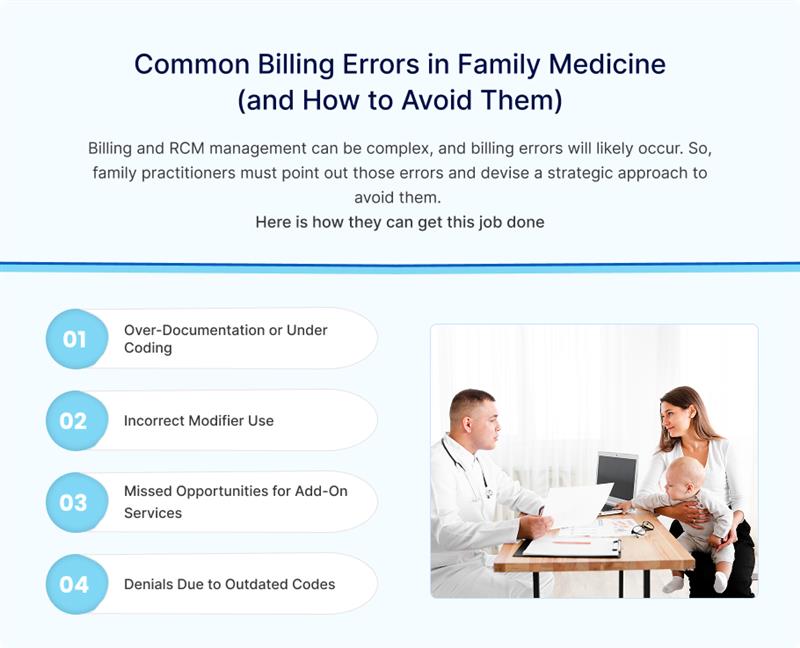
1. Over-Documentation or Under Coding
Coding occurs when a billing fails to capture all services performed during a patient visit accurately. Too much irrelevant Documentation or conservative Coding can cause immediate claim denial, repetitive tasks, resource wastage, etc.
Providers need to train staff on appropriate E/M levels and documentation standards to ensure proper coding and documentation. Use the most recent 2025 E/M recommendations to support the appropriate code levels and compare documentation to medical decision-making (MDM) or total time spent.
2. Incorrect Modifier Use
Missing or inappropriate modifiers can lead to denials.
Train staff on modifier intent and ensure correct usage for dual visits(preventive problem-focused) or telehealth services. Stay updated on payer-specific modifier rules.
3. Missed Opportunities for Add-On Services
Many practices overlook billable services such as prolonged visits, behavioral health integration, or TCM. Ensure staff is trained to capture these services accurately.
4. Denials Due to Outdated Codes
Using outdated codes can lead to denials and potential audits.
Conclusion
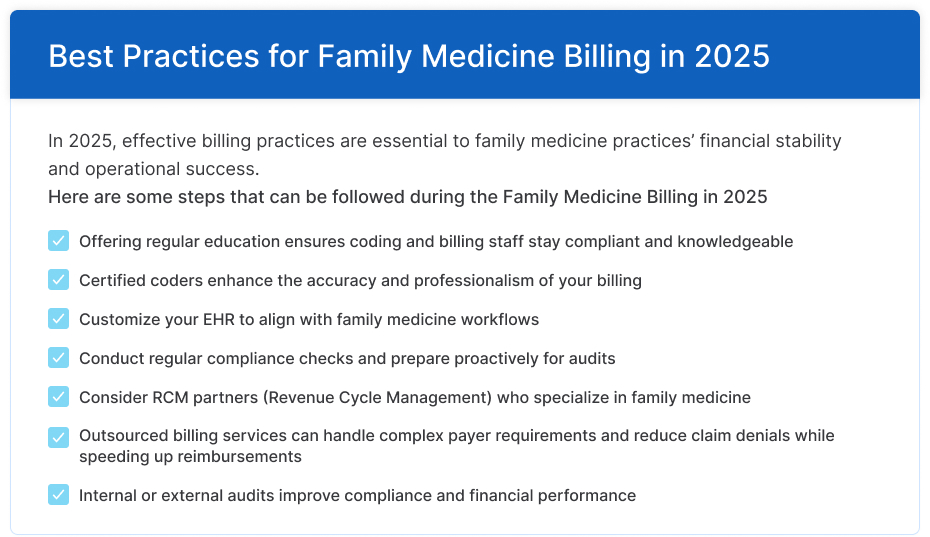
Insurance payers like Medicare and private companies often update their family medicine billing guidelines.
Healthcare practice owners need to follow these newly added changes.
It will help them reimburse the services they offer to their patients accurately and promptly.
From the reduced Medicare conversion factor to the introduction of new codes and APCM services, these changes highlight the importance of accurate documentation, proper code selection, and a deep understanding of evolving guidelines.
In 2025, the key will be to stay ahead of evolving coding systems, payer-specific requirements, and technology changes. By adopting proactive billing practices, updated coding resources, and investing in staff training, family medicine practice can maximize revenue cycles and continue to deliver high-quality services.
Are you struggling with Coding Complexity or Claim Denials?
Contact Philadelphia Medical Billing services today to learn how our expert billing support can streamline your workflow, reduce errors, and improve your revenue cycle.
FAQs
What Are the New E/M Guidelines for Family Medicine in 2025?
In 2025, New Evaluation and Management (E/M)guidelines for family medicine emphasize simplifying documentation, focusing on Medical Decision-Making (MDM) and total time spent during the encounter, and adjusting levels for specific settings like hospitals and emergency rooms. These changes streamline the coding process and better reflect the value of primary care services.
How Do I Bill a Wellness Visit and a Sick Visit on the Same Day?
To bill both a wellness visit and a sick visit on the same day, you generally need to use modifier -25 on the problem-focused visit (sick visit) code. This modifier indicates that a significant, separately identifiable evaluation and management service was performed on the same day as the preventive medicine service (wellness visit).
What Codes Are Used For Chronic Care Management in 2025?
In 2025, the principal CPT codes used for Chronic Care Management (CCM) are 99490 and 99491. Code 99490 is used for non-complex CCM. Meanwhile, 99491 is used for CCM services provided by a physician or other qualified healthcare professional, which require at least 30 minutes of personal time. Additionally, 99437 is an add-on code for 99491 and can be billed for each additional 30 minutes of clinical staff time. Finally, 99489 is used for complex chronic care management.
Is Telehealth Still Reimbursed in 2025 for Family Practice?
Yes, but reimbursement and approved codes vary. Medicare allows using standard E/M codes (e.g., 99212-99215) with modifier 95 for video and modifier 93 for audio-only visits. State parity laws affect private-payer reimbursement.